Pain Management for Military Members and Their Families
Pain is More Common and More Severe in Military and Veterans
While over a one-third of Americans suffer from chronic pain (IOM report 2011), a National Health Interview Survey published in 2016 revealed that almost two-third of veterans are in pain. Moreover, 30% more veterans than non-veterans suffer from severe pain (NHIS, 2016).
These are staggering numbers that require us to pause and reflect. Not only this is a serious problem but also requires a different approach to management compared to what civilian patients receive.
Pain is More Complicated in Military and Veterans
Majority of active-duty members and veterans who suffer from acute or chronic pain have experienced physical or emotional trauma, many also suffer from PTSD (post-traumatic stress disorder) and TBI (traumatic brain injury). When a physical injury occurs in the presence of emotional trauma, the pain becomes more strongly imprinted in our nervous system and therefore harder to treat. Even when the physical injuries heal, the “memory of it” in our brains will make the pain continue as if the physical injury never healed.

At River City Sports and Spine Specialists This is Personal to Us
Having been established in Columbus for nearly two decades, we’ve been taking care of our Military and Veterans for a long time, and we have seen first-hand the severe toll that chronic pain has on our service men and women. In addition, I grew up in a military home, and my father, JC Dawson is a Vietnam Veteran. My dad has told me many stories of trauma and pain that he and his friends in military experienced. What some of us don’t realize is that when you serve in the military, you see things that you wish you have never seen, and you don’t have to be personally harmed in order to experience trauma.
Despite the pain and struggle, my father made sure that at home he was a dad and husband first. He was and is loving, kind, strong in faith and no matter how much he may have suffered inside, he always showed us his soft, caring side, and willingness to help anyone in need. He also taught us the importance of love and peace, knowing the human toll of war and conflict. At the same time, he was there for our country when it called him to serve.
More Statistics on Pain Amongst Military and Veterans
More information about pain in veterans revealed from the NHIS survey show other concerning statistics. This information comes from questioning over 67,696 adults. Participants responded to questions about the persistence and bothersome-ness of self-reported pain during the 3 months prior to the survey. As summarized by NCCIH (NCCIH, 2016), here’s what they found:
- More veterans (65.5%) than nonveterans (56.4%) reported having pain in the previous 3 months.
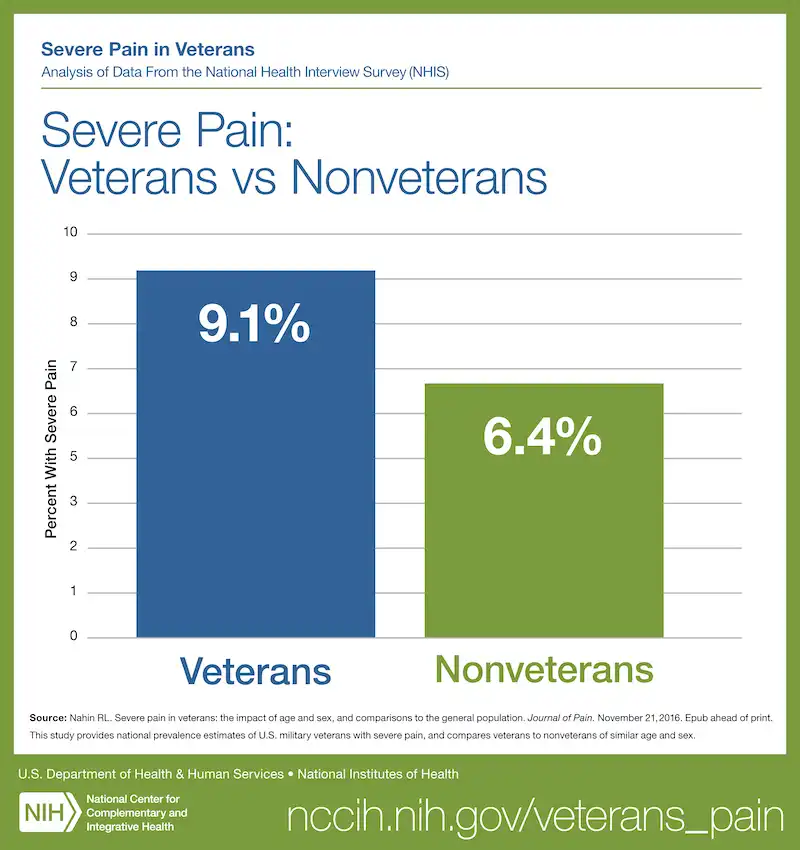
- A higher proportion of veterans (9.1%) reported having severe pain than nonveterans (6.3%).
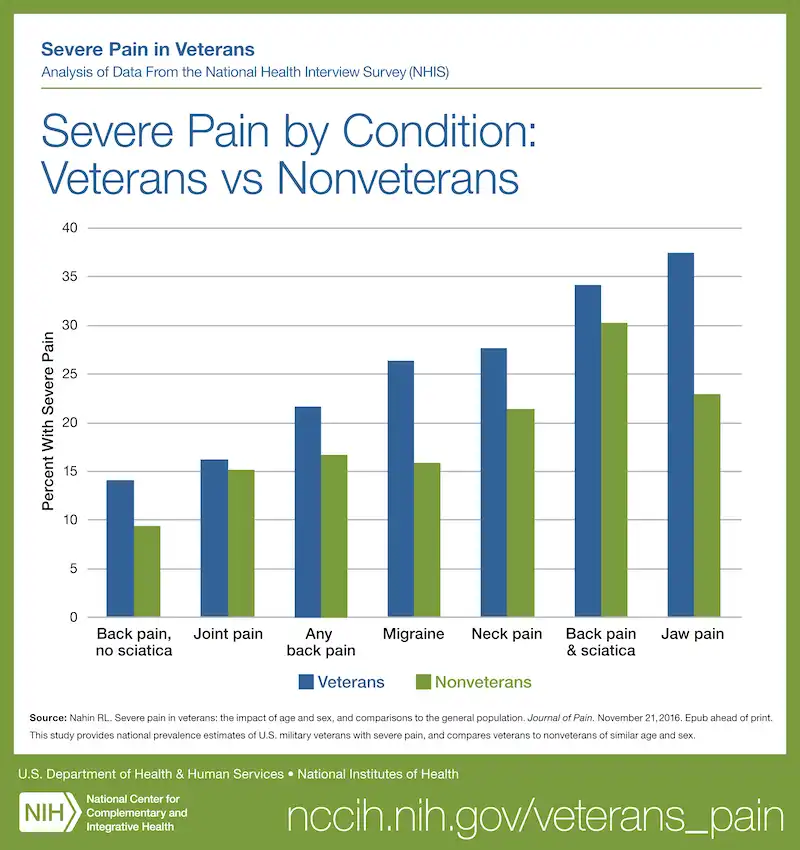
- Veterans were more likely than nonveterans to have any back pain (32.8%), back pain with or without sciatica (12.2%, 20.5%), or joint pain (43.6%), but less likely to have jaw pain (3.6%) or migraines (10.0%).
- The prevalence of severe pain was significantly higher in veterans with back pain (21.6%), jaw pain (37.5%), severe headaches or migraine (26.4%), and neck pain (27.7%) than in nonveterans with these conditions.
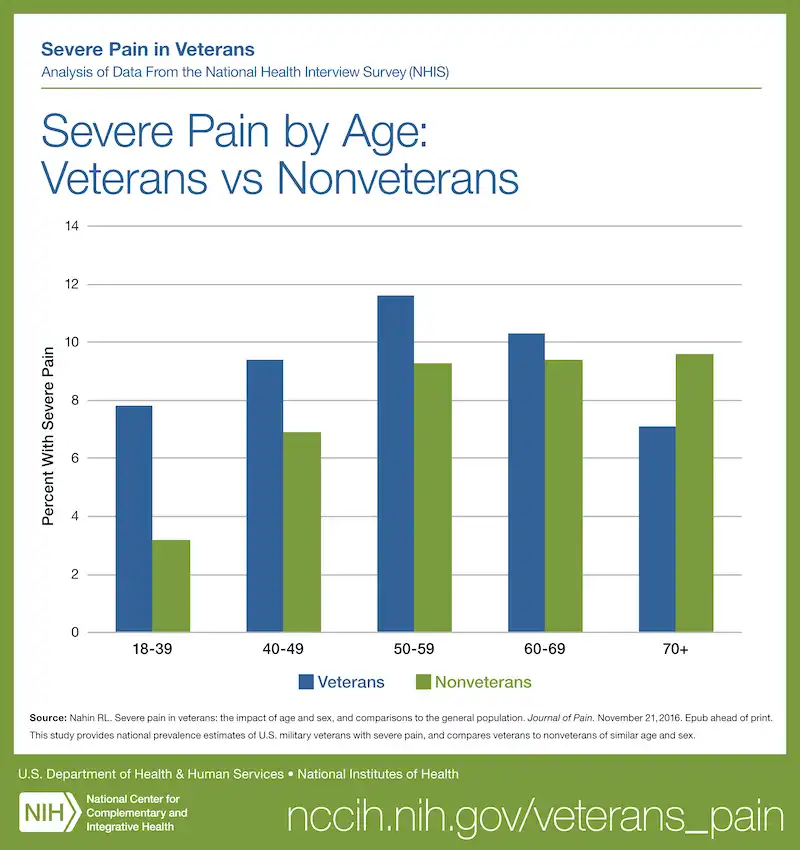
- For nonveterans, as age increased, the prevalence of any pain and severe pain also increased; however, for veterans, those aged 50 to 59 were most likely to have severe pain, while the youngest and oldest groups were least likely to have severe pain.
- Veterans aged 18-39 and 50-59 were more likely than nonveterans of the same ages to have any pain. Veterans aged 18-39 were also more likely to have severe pain than nonveterans in the same age group. However, veterans aged 70 or older were less likely to have severe pain than similarly aged nonveterans.
- Male veterans (9.0%) were more likely to report severe pain than male nonveterans (4.7%); however, no difference was seen between the two female groups
How Do We Treat Pain in Military and Veterans
 Treating chronic pain is no easy task and our military patients deserve the personalized and comprehensive care that they need. While some pain centers in the country understand the unique needs of veterans and military, unfortunately most don’t and instead, they provide the same approach as they do to their civilian patients.
Treating chronic pain is no easy task and our military patients deserve the personalized and comprehensive care that they need. While some pain centers in the country understand the unique needs of veterans and military, unfortunately most don’t and instead, they provide the same approach as they do to their civilian patients.
What we focus on at River City is first and foremost establishing an accurate diagnosis of the cause of the pain. This is obvious, as you cannot truly address the root of the problem if you don’t accurately name it first. This part of the process is not as easy as it sounds, as often times, there are a lot of “incidental findings”, such as degenerative disc disease in the spine, which may seem to explain the pain but in reality, it doesn’t. We cannot be tricked by quick explanations and need to evaluate the patient’s symptoms in a comprehensive way before coming to conclusions.
Once we find out the causes of the pain, which in most cases are multiple, our goal is to address each one of them in a targeted way. We always want to make sure that the patient is connected with appropriate resources at Ft Benning or the VA as treating military and veteran patients is always a team effort.
 In addition to that, what we uniquely offer at River City are all the standard pain management treatment modalities (such as pain injections, etc.) but also regenerative treatments (stem cells, PRP, etc.), advanced pain procedures (spinal cord stimulators, minimally invasive fusion, etc.) and a new approach to understanding how pain works.
In addition to that, what we uniquely offer at River City are all the standard pain management treatment modalities (such as pain injections, etc.) but also regenerative treatments (stem cells, PRP, etc.), advanced pain procedures (spinal cord stimulators, minimally invasive fusion, etc.) and a new approach to understanding how pain works.
We base some of our philosophy on the work of Dr. Sarno (a fellow physical medicine and rehabilitation and pain management physician) and others, who described the powerful connection between emotional and physical pain. What he described as Tension Myoneural Syndrome (TMS) is a way that our central (brain and spinal cord) and peripheral (nerves connected to muscles/ joints) nervous systems interact and create the sensation of pain that is beyond a response to tissue injury.
As physical medicine and rehabilitation specialists, our goal is to rehabilitate and restore damaged and painful tissues when possible. This is where regenerative medicine options serve us as additional tools for the right patients. Stem cells and platelet rich plasma are some of the options that we can offer, to use our own body’s healing mechanisms to restore function and strength.
References:
NCCIH. Veterans are in Pain According to Analysis of National Health Survey. 2016. Retrieved from: https://www.nccih.nih.gov/research/research-results/veterans-are-in-pain-according-to-analysis-of-national-health-survey
Institute of Medicine (US) Committee on Advancing Pain Research, Care, and Education. Relieving Pain in America: A Blueprint for Transforming Prevention, Care, Education, and Research. Washington (DC): National Academies Press (US); 2011. Available from: https://www.ncbi.nlm.nih.gov/books/NBK91497/ doi: 10.17226/13172
Nahin RL. Severe pain in veterans: the impact of age and sex, and comparisons to the general population. Journal of Pain. 2017;18(3):247-54.